Preimplantation genetic diagnosis
It is believed that genetic diseases are growing rapidly all over the world. Nevertheless, it is important to know that the number of diseases does not increase, but diagnostic capabilities become much more accessible, as well as new genetic diseases, are detected. Possibility to specify the name of the disease sometimes provides the family an opportunity to choose a specific method of treatment, but in most cases, it is only able to clarify the prognosis or anticipate the possibility of disease complications. Until now, even if the parents knew about the increased risk of genetic diseases for their offspring, it was not possible to avoid it. The earliest diagnosis for the child was possible to define during prenatal diagnostics, and if the diagnosis has been confirmed, the family faced a serious choice – to terminate the pregnancy or save, knowing that the baby will not be born healthy. Both of these decisions are complex and emotionally difficult to be accepted.
Currently, a method that allows to carry out genetic analysis of embryos before their implantation into the uterine cavity has become available in Latvia, thus avoiding the risk of certain genetic abnormalities in the offspring. This method is called preimplantation genetic diagnosis (PGD).
PGD method is being offered to families who have a high risk of genetic abnormalities in offspring, as well as if the disease-causing mutations was identified. For the family in which the child was born with a genetic disorder there are many unanswered questions. It is difficult to understand how is it possible for two healthy parents to have a baby with a genetic disease; it is not clear how high is the risk of disease for the future children in this family, and how these risks can be minimized.
To understand how genetic diseases are inherited, it should be remembered that at the moment of fusion of gametes child receives two full sets of genetic information – one from mom and one from dad. This information also brings errors (mutations), but most often, they do not affect the child’s development, and the person does not feel their presence during his lifetime because they are inherited from only one parent. Some of the mutations are lighter, the other – more severe; some manifest themselves in adulthood, the other – even before birth.
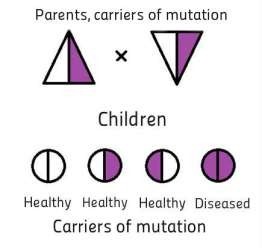
If, without knowing it, healthy parents are the carriers of a mutation in one specific gene (to anticipate this situation is almost impossible because of the huge number of genes, and the health of the carriers of a mutation is usually not changed), the child may inherit the mutation from both parents. In that case, he receives one of the so-called recessive genetic diseases.
Recessive diseases can be found separately comparatively rare, but all together they make up a significant part of all genetic disorders. In any group of people, some recessive disorders are more common, others – quite rare. The most common recessive disorders in Latvia are cystic fibrosis, phenylketonuria, recessive hearing loss, Alpha-1 antitrypsin deficiency and spinal muscular atrophy. In the case of recessive disease, the risk to inherit this disease for the next child is 25%.
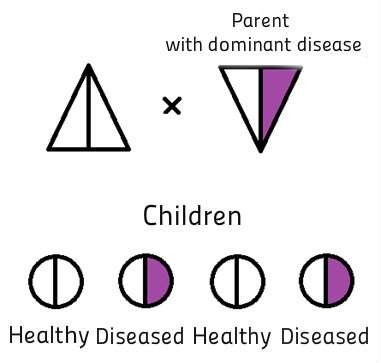
PGD method is also used in the case of genetic diseases in which there is a high risk of pathology exactly in the offspring of a particular sex. However, in such cases it is possible to make rather simple analysis, checking the chromosomes of the embryo (preimplantation genetic screening – PGS) and placing in the uterine cavity the embryo, whose sex has no risk of genetic abnormalities. Such diseases are, for example, haemophilia A and B, Duchenne and Becker muscular dystrophy, Fragile X chromosome syndrome and X-linked mental retardation.
How does this happen?
To make it possible to carry out PGD analysis, after the family received genetic counseling, blood for DNA research is collected from parents and some other family member. This stage can last up to 6 months. During that period, method of embryo cells analysis is developed individually for each family.
On the fifth day after the procedure of artificial insemination, a few cells are taken from the embryo, and the embryo undergoes vitrification (freezing). Taking cells from the embryo on the fifth day of life does not reduce the potential for its future development. The result of the analysis shows which of the embryos have inherited the mutation (-s), allowing to choose healthy ones. Additionally, preimplantation genetic screening (PGS) is carried out to ensure that the cells of the embryo placed in the uterine cavity contain a normal number of chromosomes. After carrying out this analysis, one healthy embryo is placed into the uterus to avoid the risk of twin pregnancy. If the result of the analysis showed that the family has a few healthy embryos, they will be frozen (vitrificated) and then can wait for their parents for 10 years.
If you suspect you are carriers of any genetic disease and would like to know more about IVF + PGS, contact IVF Riga Clinic for more information.